Redefining Healthcare
Virtual Care for Patient Admission and Discharge
Aprill, 2024 3:15:29 PM

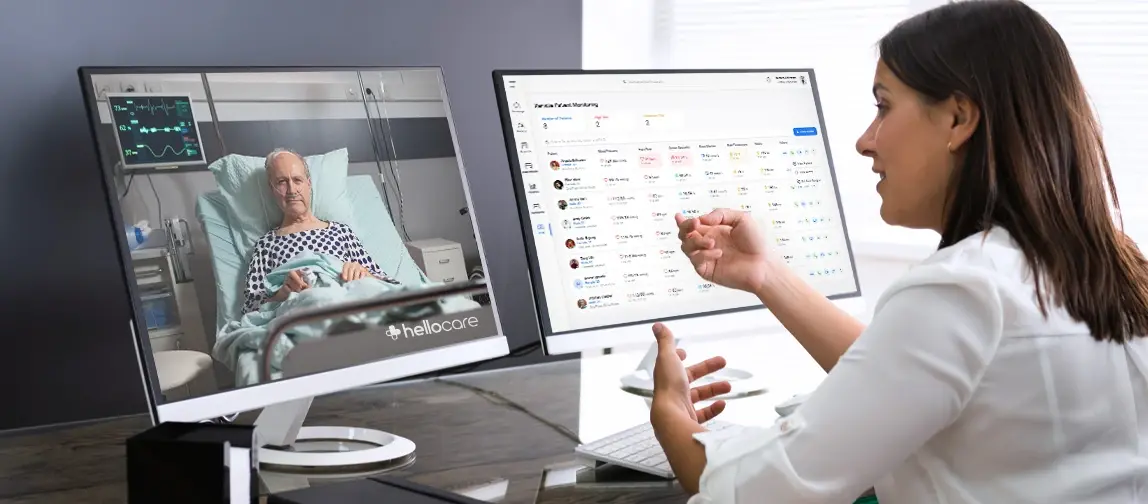
As technology continues to shape the healthcare landscape, virtual care is emerging as an essential tool
in managing patient admission and discharge processes. A 2021 report suggested that the telehealth
market,
which incorporates various aspects of virtual care, was expected to reach USD 266.8 billion by 2026 [1],
underscoring the significant shift towards digital healthcare solutions. Virtual care platforms,
particularly
those pioneered by companies like hellocare, are instrumental in this change, offering streamlined
procedures
that enhance both patient and family understanding and participation in care processes.
Traditional admission and discharge processes in hospitals are typically characterized by extensive
paperwork
and the need for coordination among various departments—from nursing to billing to pharmacy—which can be
t
ime-consuming and error-prone. This conventional method often leads to delays and a less than optimal
experience for
patients who are either eager to receive care promptly or to return home after treatment.
Virtual care technologies offer a transformative approach by digitizing and automating these critical processes. By leveraging electronic health records (EHRs) and integrated virtual care platforms, hospitals can now streamline the admission process to include automatic patient data retrieval and verification, digital consent forms, and pre-admission medical history reviews. This shift not only speeds up the process but also ensures that all pertinent information is accurate and readily available, reducing the time patients spend waiting in admissions and allowing healthcare staff to focus more on patient care rather than administrative tasks.
During discharge, virtual care systems can automate many aspects of the process, such as scheduling follow-up appointments, generating electronic discharge instructions, and ensuring prescriptions are sent directly to the pharmacy. Patients can receive their discharge instructions through digital platforms, which can include interactive elements such as videos and easy-to-understand guides on post-discharge care. This method not only minimizes paperwork but also enhances patient understanding and compliance with treatment plans, which are crucial for recovery.
Moreover, virtual care platforms can integrate decision support tools that help clinicians identify when a patient is ready for discharge, based on their recovery progress and clinical guidelines. This reduces the risk of premature discharge and helps optimize the timing of discharge to improve health outcomes and reduce readmission rates.
By reducing the administrative burden and enhancing the accuracy of patient information, virtual care technologies improve the overall efficiency of hospital operations. They enhance the patient experience at both the entry and exit points of care, leading to higher patient satisfaction and better health outcomes. This modern approach, spearheaded by innovations from companies like hellocare, marks a significant advancement in how healthcare facilities manage the critical transitions of patient admission and discharge.
Education is a critical component of the discharge process, where traditionally, the flow of information
has been predominantly
one-directional—from healthcare providers to patients. Virtual care revolutionizes this dynamic through
interactive and multimedia
educational sessions, which are facilitated by virtual nurses. These sessions include the use of
visuals, interactive guides,
and real-time feedback, ensuring that patients have a clear understanding of their health conditions and
the necessary post-discharge care.
This interactive approach not only improves comprehension but also empowers patients to manage their
conditions more effectively, which
is shown to improve adherence to treatment plans and reduce the likelihood of readmission.
Virtual care also significantly enhances the involvement of family members in the patient care process.
Through virtual meetings and access to educational content, family members who may not be able to visit
the hospital
can still participate actively in understanding and managing the patient’s condition. This inclusion
helps to bridge the
information gap between healthcare providers and families, ensuring that home care post-discharge is
effective and informed.
Research supports that greater family involvement in the discharge process can reduce patient
readmissions by up to 25%,
highlighting the importance of integrated care facilitated by virtual tools.
Transforming Admission and Discharge Procedures
Virtual care technologies offer a transformative approach by digitizing and automating these critical processes. By leveraging electronic health records (EHRs) and integrated virtual care platforms, hospitals can now streamline the admission process to include automatic patient data retrieval and verification, digital consent forms, and pre-admission medical history reviews. This shift not only speeds up the process but also ensures that all pertinent information is accurate and readily available, reducing the time patients spend waiting in admissions and allowing healthcare staff to focus more on patient care rather than administrative tasks.
During discharge, virtual care systems can automate many aspects of the process, such as scheduling follow-up appointments, generating electronic discharge instructions, and ensuring prescriptions are sent directly to the pharmacy. Patients can receive their discharge instructions through digital platforms, which can include interactive elements such as videos and easy-to-understand guides on post-discharge care. This method not only minimizes paperwork but also enhances patient understanding and compliance with treatment plans, which are crucial for recovery.
Moreover, virtual care platforms can integrate decision support tools that help clinicians identify when a patient is ready for discharge, based on their recovery progress and clinical guidelines. This reduces the risk of premature discharge and helps optimize the timing of discharge to improve health outcomes and reduce readmission rates.
By reducing the administrative burden and enhancing the accuracy of patient information, virtual care technologies improve the overall efficiency of hospital operations. They enhance the patient experience at both the entry and exit points of care, leading to higher patient satisfaction and better health outcomes. This modern approach, spearheaded by innovations from companies like hellocare, marks a significant advancement in how healthcare facilities manage the critical transitions of patient admission and discharge.
Enhancing Patient Education Through Virtual Care
Family Involvement in Care Processes
Supporting Healthcare Staff with Virtual Nursing
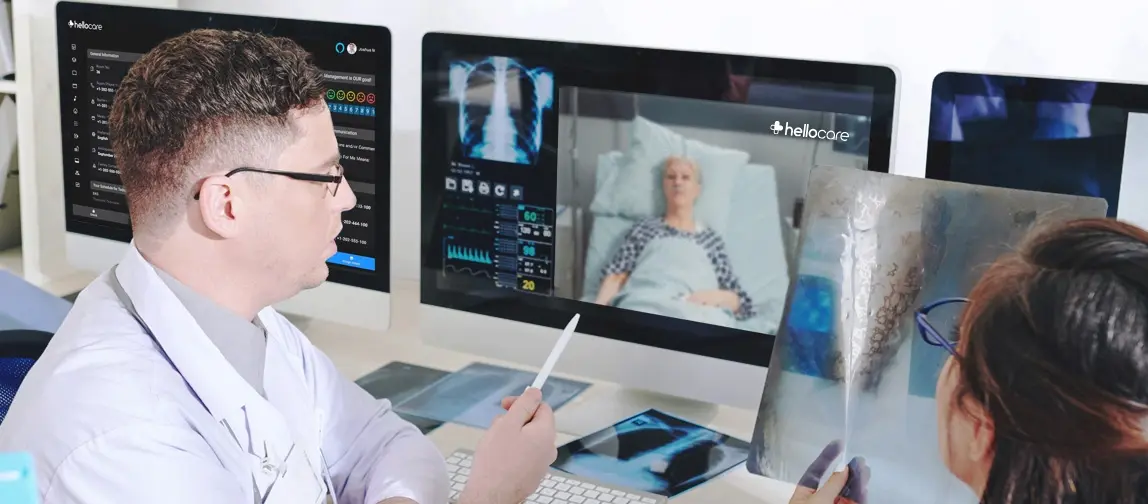
Virtual nursing is an innovative solution that addresses multiple challenges in healthcare,
including staffing shortages
and nurse burnout. Virtual nurses can manage numerous routine tasks remotely, such as patient
monitoring, initial assessments,
and pre-discharge planning. This support allows onsite staff to concentrate on direct patient care
activities, enhancing
the quality of care provided. Furthermore, virtual nursing positions are appealing to experienced
nurses seeking less physically
demanding roles, thereby retaining valuable expertise within the healthcare system. The
implementation of virtual nursing has shown
to increase job satisfaction among nurses, improve patient outcomes, and even balance the workload
more effectively across the healthcare
team.

The Future and Challenges of Virtual Care
Virtual care is reshaping the landscape of healthcare, making patient admission and discharge processes more efficient, educational, and inclusive. As this technology evolves, it holds the promise of transforming not just individual experiences but the entire healthcare system, making it more accessible, efficient, and patient-centered. As we move forward, the continuous adaptation and improvement of virtual care will be crucial in meeting the diverse needs of patients and healthcare providers alike.
Key points
- This innovative approach leverages technology to bridge physical and digital realms, creating a dynamic and personalized healthcare encounter.
- Effective communication and shared decision-making help prevent medical errors, reduce adverse events, and improve overall patient safety.
- Research indicates that patients who have positive experiences tend to be more engaged in their care, leading to better adherence to treatment plans and improved health outcomes.
- Virtual patient experience is here: Combines telemedicine, remote monitoring, and digital tools for personalized care.
80%
reduction in RN end of shift overtime
reduction in RN end of shift overtime
35%
reduction in nursing turnover based on support from virtual nurse
reduction in nursing turnover based on support from virtual nurse
350%
increase in bedside RN time spent administering medications
increase in bedside RN time spent administering medications
350%
increase in bedside RN time spent administering medications
increase in bedside RN time spent administering medications
Share
Article
Care to know more?
Request a demo to be informed about
the latest virtual nursing news and telehealth...
Related posts